What is chnnl?
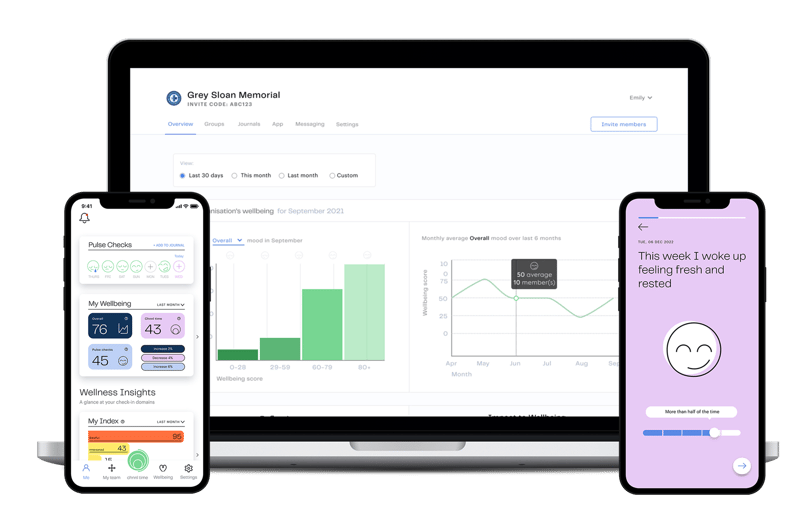
Your employee wellbeing strategy needs a tool that facilitates execution, optimisation and analysis.
Within the safety and convenience of chnnl, you can listen to your team, encourage them to engage in the wellbeing resources your company is offering, and report on their experience at work and the ROI of your wellbeing investment.
All while improving the psychological safety of your workplace.
How To Measure Employee Wellbeing?
From ESG to ISO45003, there is the global push to support employee mental health and improve the psychological safety of workplaces. And measuring and reporting on employee wellbeing is increasingly required.
The people who've been tasked with creating, executing and optimising employee wellbeing strategies need a digital solution to do so. And a realistic, humane framework for measuring employee wellbeing.
Enter our Method Of Measurement.


Analyse & optmise
Your Employee Wellbeing Strategy Tool
Our solution is made up of four groups of features that allow you to gather insights and trends from team members, encourage engagement with wellbeing resources, and report on progress and the general psychological experience at work.
Support your team and meet your health and safety compliance requirements with ease.
About us
Experts In Psychological Safety
chnnl launched after several years of backed clinical research being used as a tool by our founder Dr. Elizabeth Berryman to help manage psychosocial risks and promote better wellbeing in the workplace.

chnnl CEO & Founder Dr Elizabeth Berryman
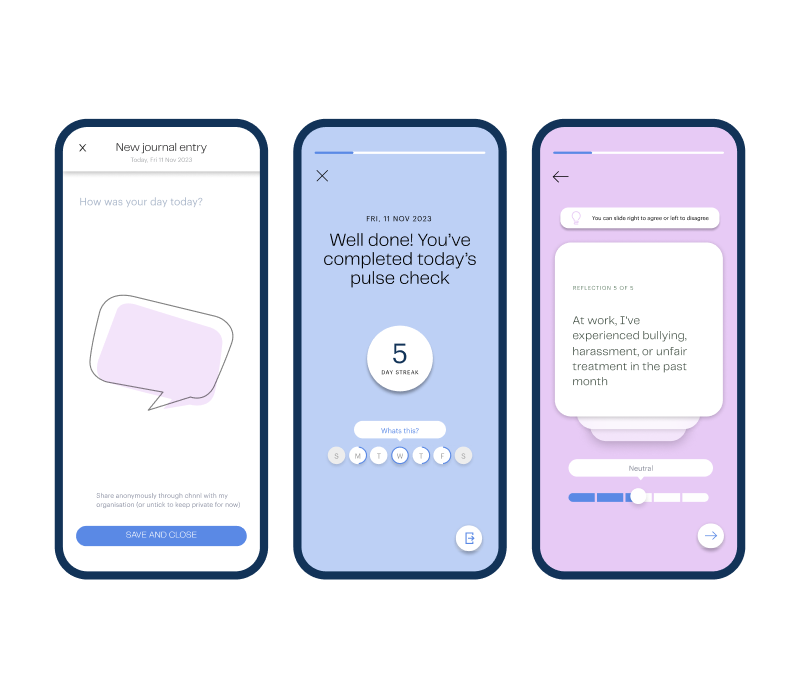
Create feedback loops for positive change
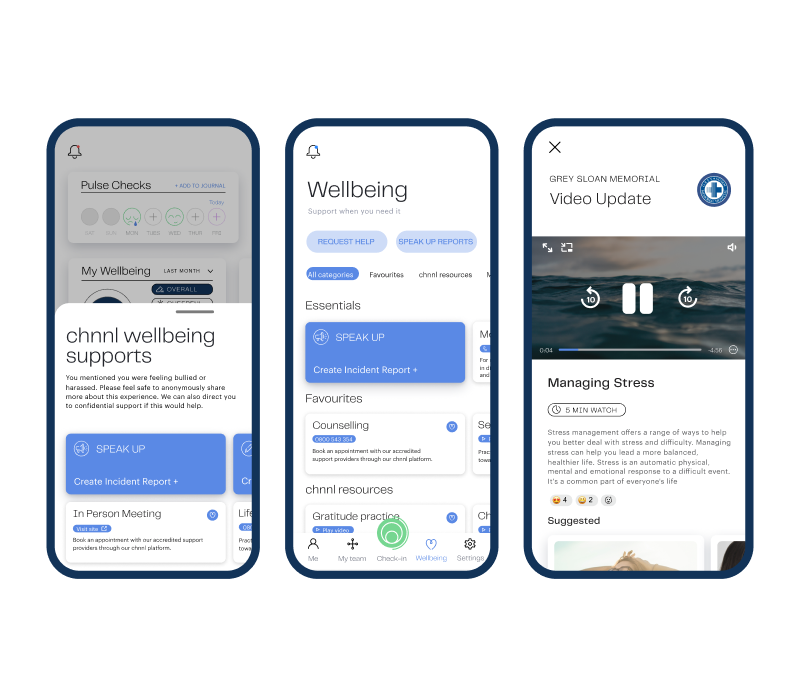
Wellbeing resources available to employees at any time


Clients using chnnl have seen
11 %
Decreased staff
turn over
2 x
Staff twice as engaged
in their work
14 %
Increased revenue
growth
11 %
Decreased staff turn over
How It Works
Case Studies
Hear from our industry leading partners who've use chnnl data to prioritise their people for best results.

-1.png?width=549&height=428&name=Blog%20%26%20Case%20Study%20Feature%20Image%20(1)-1.png)
Awards

.svg)
Intersec Awards 2023
Best H&S Product

.svg)
Winner
Top NZ Hi-Tech Awards 2021

.svg)
WINNER
Startmate Accelerator 2021

.svg)
APAC BUSINESS AWARDS
Best Mental Health Data App NZ 2022

.svg)
2022
Matchstiq Top
100 Company

.svg)
Finalist
NZ Hi-Tech Awards 2022

.svg)
Winner
NZ International Business Awards 2021

.svg)
Winner
Insider Business Awards 2022

.svg)
2021
Matchstiq Top
100 Company

.svg)
2021
NZX Early Stage Company, TIN Awards

.svg)
2021
AIHR Global Influencer in HR Tech
RELATED ARTICLES
Fresh new thinking
Keep up to date with what's new in frontline psychological safety & people-first business.
SUBHEADING
- DD MM YYYY |
- XX:XX AM |
- 6 MIN READ
- DD MM YYYY |
- XX:XX AM |
- 6 MIN READ
SUBHEADING
- DD MM YYYY |
- XX:XX AM |
- 6 MIN READ
#MakeUsSafe Campaign
Healthcare workers are on the front lines, risking their lives every day to care for patients.
Our mission is to create positive change in New Zealand healthcare organisations by taking action with data to advocate for safer working conditions.
Keep up to date with us and help us share #MakeUsSafe and let’s draw attention to this big issue, and call for change together.
.png?width=1080&height=1080&name=Untitled%20design%20(1).png)
.svg)















.svg)